FRONT PAGE
Vaccination effectiveness. What percentage of the U.S. population will have to get vaccinated to have an impact on the spread of the pandemic? Herd immunity is an end stage of a pandemic when enough of a population has developed immunity to protect the rest of the population that is not yet immune. Herd immunity stops the spread of a virus by making infection unlikely, although still possible, for those who have no immunity. Depending on the virus, herd immunity can occur when 50-90 percent of a population has achieved immunity. Anthony Fauci’s estimate of 75-85% for the coronavirus is at the high end of this scale because Covid is so highly contagious. Fauci says we won’t see any reduction in pandemic spread until around April when the population will hopefully be about 50% immune.
mRNA vaccine history and safety. The rapid development of Covid vaccines has unquestionably been shaped by political pressure and tinged with partisan influence. Has this affected vaccine safety? Not necessarily. The main reason we now have two vaccines in less than a year is that the new mRNA technology vastly reduces the time to develop and make the vaccine. Certainly the clinical trials were shorter than usual, but that shortcut allowed the FDA to issue emergency use authorizations so vaccination could start to save lives. Based on available data, the two vaccines currently in use are safe. But we won’t have a good idea about long-term safety until the vaccines have been in use for at least a year.
Does vaccination eliminate contagiousness? At the moment, we know vaccines prevent sickness, but that doesn’t necessarily mean they prevent the virus from entering our bodies and replicating for a few days. Even though the vaccine prevents the virus from overcoming our immune defenses and producing symptoms, those first few days of infection could still make us asymptomatic spreaders of the disease.
Virus mutation. The new, more easily transmitted coronavirus variant that surged positive case level in Britain has reached the U.S. We are waiting to see if vaccines will prevent it.
Covid testing. Free PCR tests are available from Marion County Health Department, CVS Pharmacy and the Indiana State Department of Health. A home test kit priced around $50 just received FDA approval and should be available soon. A $25 antibody test is available through some Kroger pharmacies.
FEATURE STORIES
I. Vaccination effectiveness
The goal of the current mass vaccination program in the U.S. and around the globe is to stop the uncontrolled spread of the pandemic. Total eradication of the virus is unlikely. But if virus spread can be reliably contained, the economically and psychologically damaging lockdowns can be lifted on a more permanent basis. Dr. Anthony Fauci predicts that the U.S. will contain the virus spread through herd immunity when about 80 percent of the population has been vaccinated.
Herd immunity defined. The concept “herd immunity” emerged from the observation that once a certain percentage of a population achieves immunity, that “critical mass” of immunity will stop the disease from spreading to vulnerable people due to the scarcity of new hosts to infect.
People without immunity can still be infected, but their risk of infection is vastly lowered. Some public health scientists prefer the term “herd protection” since this phenomenon does not actually give immunity to anyone.
If a person does get infected, the disease will not spread in an “outbreak” fashion. The “R” value, or reproductive rate, of the disease will be close to zero.
Can our government use herd immunity as a tool to stop the pandemic? The scientific community is unified in advising against a public policy allowing an infectious disease to spread intentionally in order to achieve herd immunity. The possible benefit in quicker end the pandemic could not justify the inevitable cost in the massive number of lives lost.
Instead, it recommends using mass vaccinations to reach the critical mass of herd immunity. Anthony Fauci estimates that critical mass will occur when 75-85 percent of the population have been immunized with vaccines sometime in the second half of 2021.
Factors affecting vaccine success. However, Dr. Fauci’s hopeful prediction depends on many factors. Foremost is for enough people to be willing to be vaccinated to reach the 75-85 percent threshold. Another key factor affecting vaccination effectiveness is the length of time vaccines will sustain immunity.
Unfortunately, no one knows how long immunity will last because the vaccine testing requirement was shortened to allow emergency FDA authorization. Historical data has shown that immunity from other coronaviruses generally lasts for 6 months to 2 years. Immunity against reinfection from the current SARS-CoV-2 coronavirus will be at least 6-11 months since reinfection has been so rare. Reinfection apparently has occurred in less than 1 percent of positive Covid cases over the 11-plus month course of the pandemic.
Cultural and historical resistance to vaccines.
…Trayvon Martin’s mother, Sybrina Fulton, who last month ran for a county commissioner’s seat in Florida’s Miami-Dade County, posted her doubts on Instagram, asking, “I really want to trust the scientist but why do they have a vaccine for COVID-19 so fast but not cancer or AIDS?” –The New Yorker, December 19, 2020
Any segment of the population that has felt disenfranchised, excluded, or misused by the U.S. government—in other words, most non-white Americans—can justifiably feel concerned about Covid vaccine safety. The political motives behind the government’s Operation Warp Speed to hasten vaccines to regulatory approval only add to the suspicions.
Several key facts need to considered, however, when weighing possible benefits against possible risks.
1) The highly efficient nature of the mRNA technology, compared to conventional vaccines, reduces the time required for vaccine development and production. While they may at first sound more complex, the processes involved in finding and then creating a potent mRNA vaccine are simply more direct and much faster than the older methods of making effective vaccines.
2) mRNA vaccines have a substantial history dating back to 1990. So, researchers have had decades to understand the risks and work on minimizing or eliminating them.
3) We know that mRNA cannot enter the DNA of our cells
4) We know that mRNA is quickly destroyed by enzymes after it has done its work of giving our cells the blueprint, the template actually, for making protein antigens that activate our immune systems.
To summarize, it is not surprising that we now have two effective mRNA vaccines because mRNA technology enabled vaccine companies to develop and make the vaccine in less than half the time required for conventional vaccines. It is only the period for testing vaccines that has been shortened. The FDA issued its “Emergency Use Authorization” for the current vaccines because that designation doesn’t require the longer clinical trials that full FDA approval requires.
The next story in this issue of CovidGram explains mRNA technology in detail. As with most major innovations in medicine, there are risks to consider. CovidGram attempts to give readers the best information available about mRNA vaccines.
References
Nature, October 21, 2020, The false promise of herd immunity
https://www.nature.com/articles/d41586-020-02948-4
OSF Preprints, August 6, 2020, Covid and false dichotomies
https://osf.io/k2d84/?trk=organization-update_share-update_update-text
NPR, December 24, 2020, Worst over for Manaus?
https://www.npr.org/sections/goatsandsoda/2020/12/24/949799132/the-worst-of-covid-should-be-over-for-one-hard-hit-brazilian-city-but-its-not
II. mRNA vaccine history and safety
First, a serious introduction to mRNA. The currently available mRNA vaccine got its name because it injects molecules of coronavirus-specific mRNA into your body. Those molecules direct your cells to manufacture large quantities of the coronavirus spike protein, which in turn spur your immune system to start its own personal “Warp Speed” program of making antibodies to destroy anything with a coronavirus spike on it.
The better you understand the mRNA molecule in its many forms, the better you will be able to make informed decisions about any risk involved in mRNA vaccines. So, fasten your seat belts for a lightning quick tour through the essentials of molecular biology. If you have no appetite at all for a biochemistry lesson, skip down to the subheading mRNA, viruses, and vaccine safety.
Two vital biomolecules: mRNA and proteins. The idea of using mRNA to make vaccines for various diseases is not new. Thirty years ago, researchers began synthesizing different mRNA molecules to direct cells to make specialized parts of flu, rabies, and other viruses for vaccines. mRNA molecules have been around much longer, by several million years.
The long history of mRNA molecules suggests they probably play an important biological role. In fact, they enable cells to make the many thousands of protein varieties needed to run the complex business of the living human organism. Our cells use collagen to build connective tissue, keratin to make hair, hemoglobin to transport oxygen in our blood, and immunoglobulin to make immune system antibodies, to name just a few of the better known proteins. mRNA is essential to protein synthesis.
Carrying genetic information. mRNA is a type of single-stranded molecule that chains together four basic components—four nucleotide bases abbreviated as A, U, G, and C—in a long string combining copies of these four bases in a specific sequence. Those hundreds or thousands of As, Us, Gs, and Cs, combined in what might appear to be a random order, represent the specific code for making each different protein in our bodies.
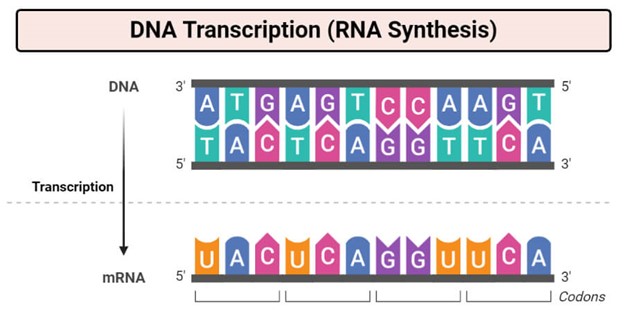
This is how the genetic code works. Each protein has its own particular sequence, therefore its own particular mRNA molecule custom made for that protein in a process called transcription (see diagram above). Living up to its name—the “m” stands for “messenger” RNA—the mRNA takes the code for a particular protein from one or more genes in our DNA and carries it out of the cell’s nucleus to the protein-making machinery in the cytoplasm. (For those of you familiar with DNA’s composition of A, T, G, and C bases, these are the same bases that make up mRNA, except mRNA uses U bases instead T bases.)
Proteins are strings of amino acids. Protein-making machinery starts at one end of the mRNA strand and reads the long string of nucleotide bases three at a time. For every triplet of bases, it spits out a particular amino acid. Proteins, which consist of long amino acid chains, are assembled this way, one amino acid at a time. Each of the 64 possible triplet combinations of A, U, G, or C bases is a code, or codon, for one of the 20 fundamental amino acids.
As the genetic codebook in the table below shows, most amino acids can result from more than one codon. The table identifies amino acids by the colored dots containing the first letters of the amino acid names. The base triplet UUC, for example, codes for the amino acid phenylalanine shown as the orange dot labeled “Phe”.

mRNA, viruses and vaccine safety. The preceding bonus lesson in molecular biology was a roundabout way to demonstrate how closely connected mRNA is to proteins and how essential that connection is to life. In other words, mRNA is no stranger to our bodies and by itself should raise no safety concerns. But what about laboratory-made mRNA that directs our cells to make coronavirus spikes?
mRNA exists everywhere proteins are made, which is in every system, organ, and cell in our bodies and the bodies of every living thing…except viruses. Viruses are so small and basic that they don’t have protein-building machinery. Instead, when they infect a host like us, they commandeer our cells’ machinery using viral RNA to make the proteins necessary to replicate themselves.
The coronavirus mRNA vaccine mimics a virus invasion by directing our cells to make coronavirus spike protein. The presence of spike proteins then mobilizes production of antibodies. But, fortunately for us, the vaccine accomplishes that task without using virus RNA. Vaccine companies can put together in the laboratory any desired mRNA for the production of any protein.
Making mRNA in the lab, to order, is relatively easy. Since the late 20th century, researchers have been able to custom make mRNA in the laboratory. Starting around 1990, vaccine companies harnessed the simplicity of making mRNA to experiment with its potential to produce encoded proteins in vivo, inside living animals. Just like naturally produced mRNA, they found that synthetic mRNA injected into live tissue could induce cells to produce the desired protein.
Since then, vaccine companies have lost no time refining mRNA vaccines through various chemical processes to produce antigens for specific diseases which, in turn, would induce cells to produce appropriate antibodies against those diseases such as flu, rabies, zika, and cytomegalovirus.
Safe by scientific consensus. mRNA vaccines are considered safe from the possibility that their RNA could be integrated into human DNA. Scientific dogma holds that RNA “cannot integrate into genomic DNA without the presence of…[retrovirus enzymes]”, which can reverse the ordinary direction of genetic transcription. However, a 2001 paper in Genome Biology reported that 8 percent of the human genome consists of retrovirus-like sequences that have accumulated over the human history of exposure to retroviruses.
Does this finding raise the possibility of a reverse transcription risk? The scientific consensus concludes that the possibility of reverse integration of vaccine-based RNA is so remote in theory that there is no actual risk and that we should focus safety concerns on other possible risks.
So far, the Pfizer-BioNTech and Moderna vaccines have proven safe under the conditions spelled out in a recent CDC bulletin. For persons susceptible to extreme allergic reactions, as have been reported in isolated cases, the CDC recommends caution and advises weighing the vaccine benefits against the potential risks.
References
Horizon, December 11, 2020, Five things you need to know about mRNA vaccine safety
https://horizon-magazine.eu/article/five-things-you-need-know-about-mrna-vaccine-safety.html
Vaccines, April 24, 2019, Comparison of plasmid DNA and mRNA vaccines
kheprw.org/wp-content/uploads/2020/11/liu2019-comparison-of-plasmid-DNA-and-mRNA-as-vaccine-technologies.pdf
New England Journal of Medicine, December 10, 2020, Safety and efficacy of Pfizer vaccine
https://www.nejm.org/doi/full/10.1056/NEJMoa2034577?query=RP
NIH, August 23, 2020, Prospect for SARS-CoV-2 spike protein in vaccines
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7443330/
III. Does being immunized against Covid mean the virus cannot enter our bodies? Does it mean we cannot infect other people who are not yet immunized?
Not necessarily. Because of the shortened clinical trials, we don’t know enough about the interaction of the vaccine and the virus to say that the Pfizer-BioNTech and Moderna vaccines will completely prevent infection. This statement might be confusing since the vaccine does prevent Covid. It prevents Covid symptoms. So why can’t we also say it prevents infection?
By “infection” we simply mean that the virus starts to enter our bodies and begins to replicate. During the first few days of this coronavirus infection, the virus is spreading in our bodies without producing symptoms. In the graph below, the gray curve tracks the amount of virus in the body, the “viral load”. The infection starts at day “-5” (negative 5), when exposure to the virus occurs.

Days elapsed
For this new coronavirus, an infection takes time to spread in the body and overtake our defenses before we start to see symptoms. In this context, we don’t say that an infection has produced illness, or disease, until it produces symptoms. If you are vaccinated, the virus won’t produce symptoms; it won’t make you sick. But you could still have enough virus in you to shed some onto others and spread the disease.
Most familiar diseases like the flu track closely with the course of infection. If you are infected with the flu, you are sick with the flu. You have the symptoms. And you are contagious. It’s different with Covid.
If the vaccines do not prevent a minor infection—that is, they allow the virus to replicate, but not enough to cause symptoms—then vaccinated people could still be harboring enough virus to spread the disease.
References
NPR, November 30, 2020, Moderna vaccine gets more good news
https://www.npr.org/sections/health-shots/2020/11/30/940037920/more-good-news-for-modernas-covid-19-vaccine-candidate
NPR, December 18, 2020, I felt fine but tested positive
https://www.npr.org/sections/health-shots/2020/12/18/947407917/i-felt-fine-but-tested-positive-for-the-coronavirus-whats-that-really-mean
NPR, December 4, 2020, What to do if you test positive this winter
https://www.npr.org/sections/health-shots/2020/12/04/939050215/what-to-do-if-you-test-positive-for-the-coronavirus-this-fall-or-winter
NPR, December 12, 2020, What you need to know about vaccines
https://www.npr.org/sections/health-shots/2020/12/12/945288710/what-you-need-to-know-as-the-first-covid-19-vaccine-heads-your-way

